Introduction
It has been well studied that immune dysregulation in autoimmune diseases is a risk factor for the development of Non-Hodgkin's lymphoma (NHL). However, the underlying mechanisms are not well understood. Although certain traditional risk factors like prolonged immunosuppression, infections, advanced age, family history, and history of organ transplantation are well described in NHL patients, there is limited literature regarding their interplay with autoimmune diseases. Hence, we conducted this retrospective study from the National inpatient sample database to describe the various clinical and demographic factors that increase the risk of NHL development in patients with autoimmune diseases.
Methods
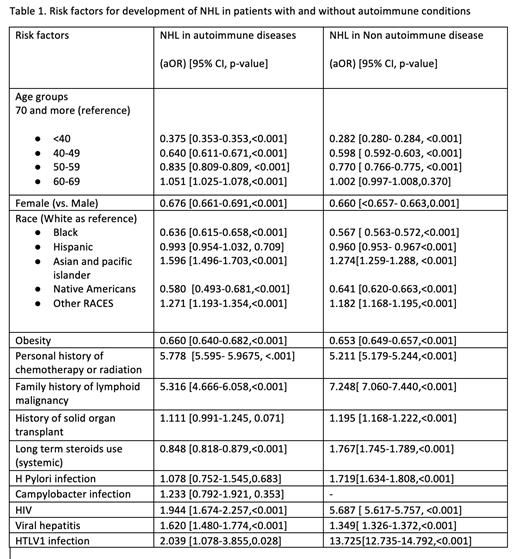
Our study was conducted using the National Inpatient Sample, which is a large all-payer inpatient care database in the United States. We collected data from 2016-2020 on all adult patients aged > 18 years who had NHL. We divided them into two cohorts: one with underlying autoimmune diseases and one without underlying autoimmune conditions. We then compared the adjusted odds ratios (aOR) of various risk factors like age, race, gender, obesity, family history of lymphoproliferative diseases, personal history of chemotherapy or radiation, history of HIV, HTLV-1, Helicobacter pylori infection, Chlamydia infection, history of solid organ transplantation, and long-term steroid use among the two cohorts.
Results
Our data initially consisted of 148,755,036 patients ages ≥18 years, with 4,291,559 cases having autoimmune disorders like rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), Systemic sclerosis, sarcoidosis, sjogren's syndrome, and celiac disease. We found that 0.9% of autoimmune cases had NHL, while 0.7% of non-autoimmune cases had NHL (aOR 1.272, 95% CI 1.258-1.285, p<0.01). Among those with autoimmune conditions, various factors also influenced the presence of lymphoma, such as personal history of chemotherapy or radiation (aOR 5.778, 95% CI 5.595- 5.9675, p <0.001), family history of lymphoid malignancy (aOR 5.316, 95% CI 4.666-6.058, p<0.001), HIV infection (aOR 1.944, 95% CI 1.674-2.257,p<0.001), advanced age of 60-69 years (aOR 1.051, 95% CI 1.025-1.078, p<0.001) , Asian and Pacific Islander ethnicity (aOR 1.596, 95%CI 1.496-1.703, p<0.001) and viral hepatitis (aOR 1.620, 95% CI 1.480-1.774, p<0.001) (Table 1).
Conclusion
The increased risk of non-Hodgkin Lymphoma (NHL) with autoimmune conditions like rheumatoid arthritis and SLE is well established. Studies have also shown that these patients can overall have a poor prognosis from their NHL when compared to patients without autoimmune diseases. However, there is limited literature regarding the interplay of traditional NHL risk factors with underlying autoimmunity. Hence, our retrospective analysis sheds light on the lesser studied risk factors, such as patient characteristics and comorbidities. We found that older age, male sex, Asian and Pacific Islander race, family history of lymphoid malignancy, personal history of chemotherapy or radiation, and comorbidities like HIV, Viral Hepatitis, and HTLV-1 are some strong risk factors associated with the development of NHL in patients with autoimmune diseases. Infections like HIV and HTLV-1 played less of a role in the autoimmune cohort as opposed to the non-autoimmune cohort. Whereas personal histories of chemotherapy and radiation and family histories of lymphoid malignancies were demonstrated to be very strong risk factors in both settings.
Hence, our study enables clinicians to identify the differences in the interplay of these risk factors and to perform stringent monitoring of patients when they do have these risk factors
Disclosures
No relevant conflicts of interest to declare.